Thermography
Medical Thermography
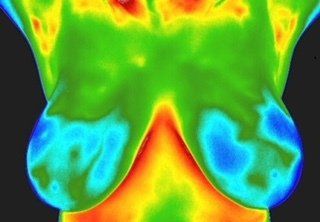
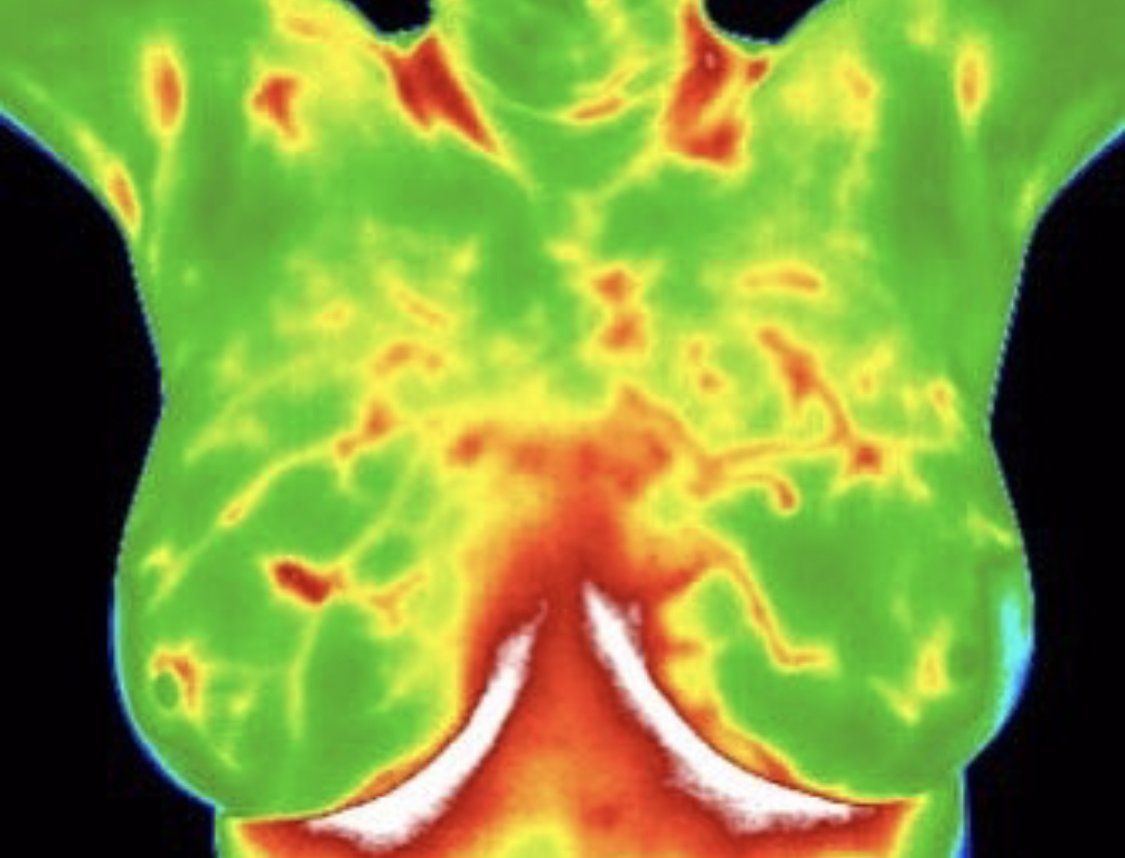
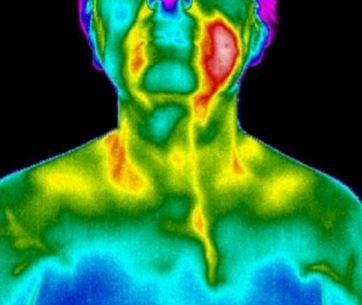
Thermography measures the infrared radiation (heat) which emits from the surface of the body, revealing subtle variations that may indicate areas of dysfunction. Depending on the metabolic activity, areas of concern may appear either warmer or colder than surrounding tissue. A highly sensitive medical infrared camera and advanced software convert this heat data into a visual image known as a thermogram.
These images are analyzed by Board Certified Thermologists-physicians specially trained to interpret thermal patterns-who provide a detailed report of the findings. Thermography has been used for decades and is a valuable tool for identifying physiological changes in the body.
While thermography is widely recognized for its role in breast health screening, it also has many other applications due to its ability to detect inflammation-often a precursor to conditions such as cardiovascular disease, diabetes, arthritis, and more. Whether evaluating the lymphatic or vascular systems, or focusing on specific areas like the oral cavity, thyroid or breasts, thermography takes a holistic view of the body as an interconnected system.
A thermography screening can assess the health of the thyroid, oral cavity, breasts, abdomen and lower body as well as any other areas of concern. Because it is non-invasive and does not involve X-rays or physical contact, thermography is ideal for routine wellness screenings. It can help detect physiological changes, offering a to make preventative lifestyle adjustments though diet, supplementation, stress management.
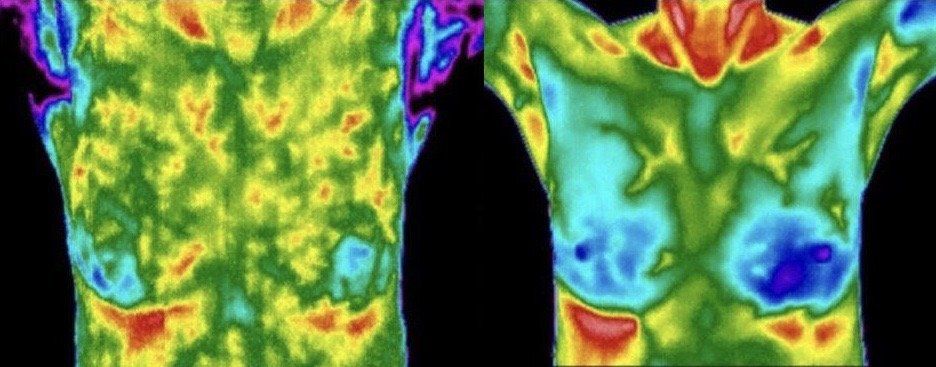
For example on patient was found to have a hormonal imbalance following her initial thermography screening. With guidance from her physician, she implemented dietary changes, and supplementation. Just six months later, her comparison screening showed significant improvement-reflecting not only enhanced thermal patterns but also improved overall health .
In a healthy body, thermal symmetry (evenness of temperature from one side to the other) is expected. This "thermal fingerprint" remains stable over time. When an imbalance or dysfunction occurs, asymmetry may develop, signaling the need for further evaluation. Thermography is patricianly effective when a baseline screening is followed by routine comparisons.
It is essential to follow the recommendations outlined in your thermography report, especially when it comes to the timing of follow-up or comparison screenings. These steps help ensure accurate monitoring and provide the opportunity for timely, proactive care.